Evelynn Hammonds, a historian of science at Harvard, said, “There has never been any period in American history where the health of Blacks was equal to that of Whites. Disparity is built into the system.” (1)
By any and every measure, there are vast differences in healthcare access and outcomes when comparing Black and White Americans. 2015 data from the CDC shows, life expectancy is lower among Black Americans by about 3 years and by almost 6 years for Black males. Racial disparities in healthcare also exist for Latinx communities. The Kaiser Family Foundation (KFF) cites great differences in those without health insurance, even after the implementation of the Affordable Care Act in 2010. For example, in 2018, 7.5% of White Americans were uninsured compared to 19% of Hispanic Americans and 11.5% of Black Americans.
“Despite being recognized and documented for many years, disparities in health and health care have persisted and in some cases widened over time. KFF analysis finds that Black and American Indian or Alaska Native individuals continue to fare worse compared to White individuals across most examined measures of health status, including physical and mental health status; birth risks; infant mortality rates; HIV and AIDS diagnosis and death rates; and prevalence of and death rates due to certain chronic conditions.” (2) These disparities are symptoms of broad, systemic social inequities in our society, including structural and systemic racism.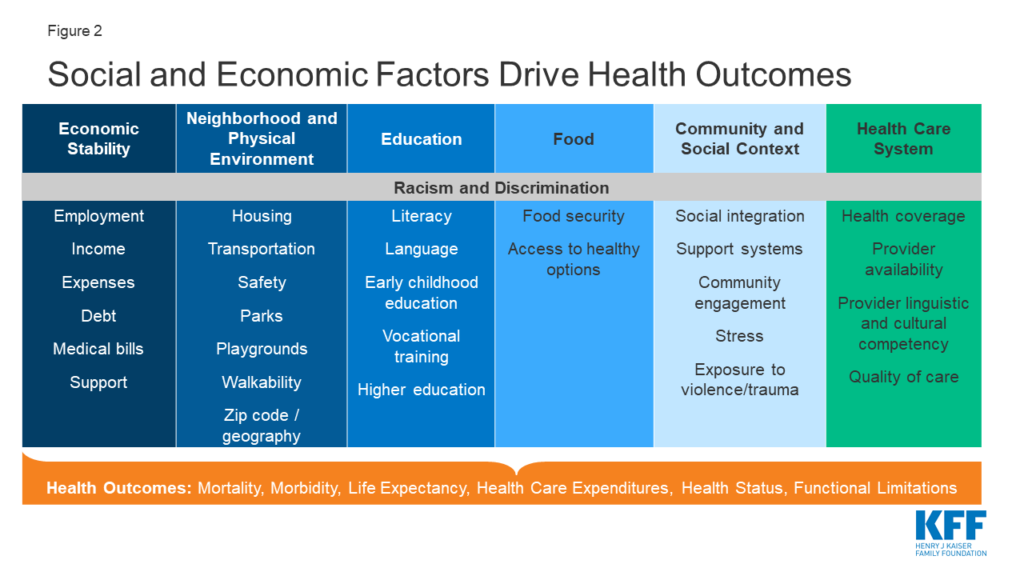
The COVID-19 pandemic has magnified and exacerbated these injustices. The impacts of the pandemic on people of color in the U.S. has been profound. For the majority of states reporting data, Black people account for a higher share of COVID-19-related deaths and cases compared to their share of the population. Similarly, Latinx individuals make up a higher share of confirmed cases relative to their share of the population and there have been strikingly disproportionate impacts for American Indian or Alaska Native, Asian, and Native Hawaiian or Other Pacific Islander communities in some states. (3) Per capita In Illinois, there are about 9,633 COVID-19 cases per 100,000 Latinx Illinoisans compared to 5,811 cases per 100,000 White Illinoisans, based on the U.S. Census and Illinois Department of Public Health data. (4) Additionally, the rate of vaccinations is lower for people of color than for White people. (3) (5)
Due to historical systemic racism, it is no surprise to learn that Black Americans may be reluctant to trust the American medical establishment. This mistrust is due to various unethical medical programs and studies, among them the horrific Tuskegee Syphilis Study which was conducted by the United States from 1932-1972, using Black men to study the effects of untreated syphilis. This mistrust adds to the social and economic factors resulting in poor health outcomes. (1)
What can we do to fight for equity in health care and health outcomes?
- Advocate for quality, universal health insurance that is available regardless of employment status, income level, and employer.
- Fight for racial justice in all aspects of life.
- Promote educational policies that will increase the number of BIPOC doctors.
- Continue to learn more about racial inequities.
Sources
- https://www.nytimes.com/2020/01/13/upshot/bad-medicine-the-harm-that-comes-from-racism.html?
- https://www.kff.org/policy-watch/health-disparities-symptom-broader-social-economic-inequities/
- https://www.kff.org/coronavirus-covid-19/issue-brief/latest-data-on-covid-19-vaccinations-race-ethnicity/
- https://www.dailyherald.com/news/20210217/how-bensenville-is-tackling-high-covid-19-rates-among-hispanic-residents?utm_source=morning%20alert&utm_medium=email&utm_content=article%20column&utm_campaign=Morning%20Alert%202%2F17%2F2021
- https://www.nytimes.com/2021/02/18/world/us-coronavirus-vaccine-minorities.html?campaign_id=154&emc=edit_cb_20210218&instance_id=27261&nl=coronavirus-briefing®i_id=54064892&segment_id=51928&te=1&user_id=930e5a7654c1a2ba0991f4069592a493
